The Work and Pensions Secretary, Mel Stride, recently stated that getting back to work is “good for mental health”, and many people who have been supported well by Individual Placement and Support would agree with him. We know that work – when it’s in a supportive environment, with accommodations for mental health needs such as flexible and remote working, understanding managers and paid time off for health appointments, can support people’s mental health both directly and by reducing the negative impacts of poverty. But this is not always true. Toxic workplaces are very bad for mental health, and de-personalised approaches to getting people back into any kind of work that they might just be able to do – regardless of whether it improves or worsens their mental health – is no good for individuals, employers or the cost-effectiveness of supported employment provision.
Individual Placement and Support (IPS) is a proven and effective method of providing help for people with health conditions to find the right job and succeed in it. IPS was initially trialled in the 1990s as an approach specifically for people with long-term or severe mental illness (SMI).
Centre for Mental Health has worked at the forefront of research and policy to establish IPS in the UK. We also implemented a highly successful pilot to establish new IPS services in six mental health trusts across the length and breadth of England, which demonstrated the importance of high quality training, and the integration of employment support within multi-disciplinary mental health teams.
Building on the national evidence
Over the last six years, NHS England has substantially invested in funding IPS to increase the number of employment specialists available to work with people accessing secondary mental health services. This funding has increased year on year as part of the Government’s commitment to ensuring that IPS is widely available in mental health trusts.
Alongside this, a number of newer services, usually funded at least partly by DWP, have begun working with people accessing health services in primary care. In addition, a randomised control trial for IPS within Drug and Alcohol treatment teams demonstrated effectiveness, leading to a national roll out of IPS-AD (IPS – Alcohol/Drugs) services, led by local authority commissioners.
The IPS fidelity scale
IPS services are rated against a fidelity scale, which was created to help commissioners and providers ensure that new services adhere closely to the same quality as the original evidence-based model. This fidelity is key to achieving paid work outcomes for at least 40% of people supported. One of the crucial elements of fidelity is integration with health support. The employment specialist works within a multi-disciplinary team, which addresses people’s needs holistically. A detailed ‘return to work’ plan is created collaboratively by the client and their employment specialist, working at pace to seek out a job which matches a person’s needs (including their social, health and financial needs), their skills, preferences and ambitions, and provides job satisfaction for the right number of hours per week. That might sound like a lot of trouble to go to in order to get one person into work, but it’s why IPS is so successful: caseloads are small and employment specialists have excellent people skills which they use to build trust with clients and with each employer they meet.
The expansion of the IPS family
Where once IPS was only available to people in secondary mental health services, it is now offered across a range of settings.
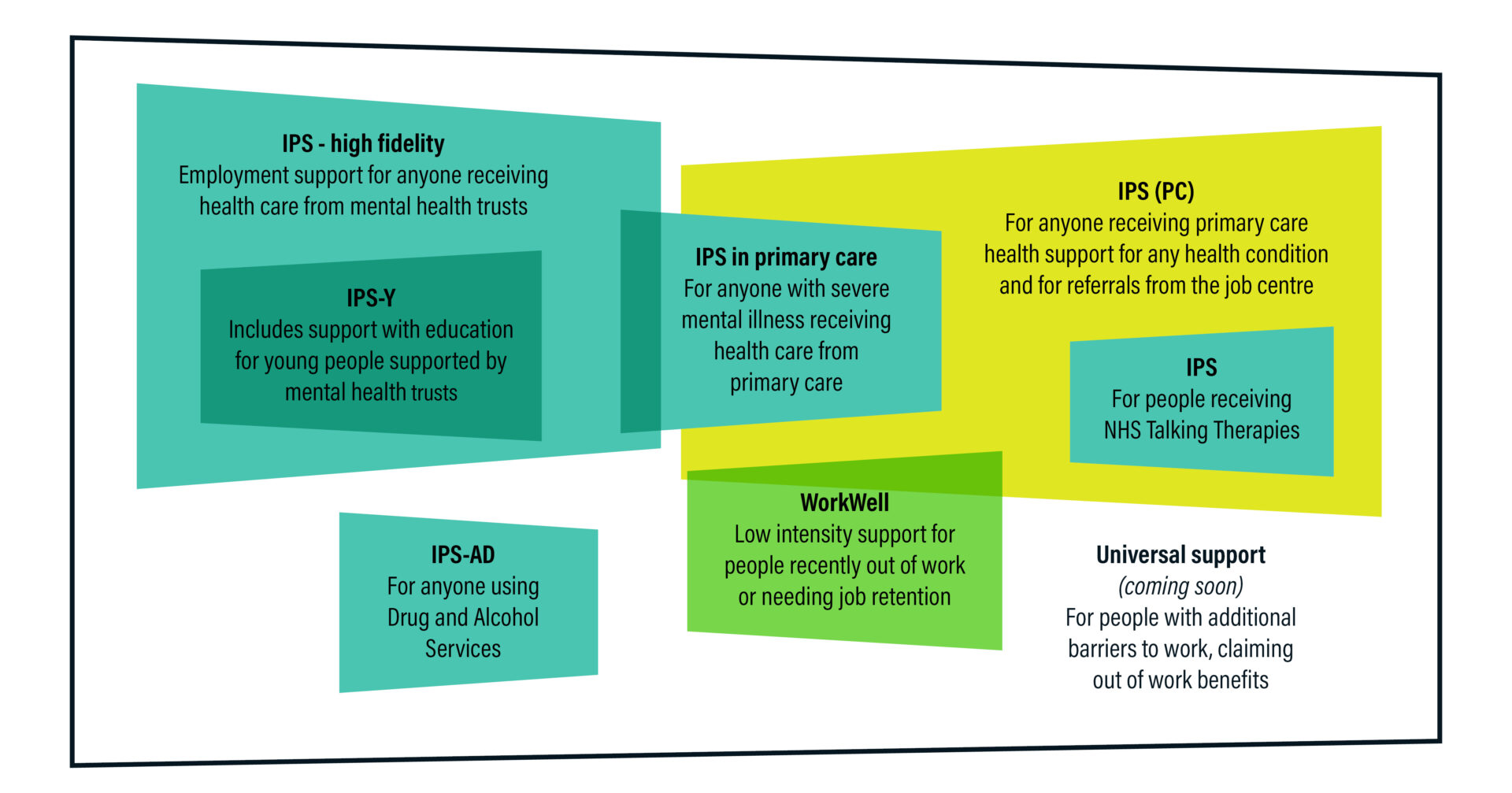
This diagram shows the current IPS landscape: the client group that IPS is funded to help, and where each service sits. There are a large number of different providers of IPS, including NHS mental health trusts, national and local charities, housing associations and national employability companies. They are funded differently for different groups of people, and it remains to be seen whether they will all be as effective as each other.
Are all employment services basically the same?
No. Having trained IPS providers and supported services for over a decade, Centre for Mental Health has confidence only in provision which achieves high fidelity to the IPS model, i.e. where services are scored at ‘good’ fidelity when assessed.
In our experience, services which omit some of those factors of quality will only support a small percentage of people – those with the least complex barriers to work – through a conscious attitude of ‘cherry picking’ to achieve quick wins. The more expensive, but more successful traditional IPS services will:
- Have caseloads of under 25 people
- Not only take referrals from health colleagues, but work together with them, ensuring that interventions for work and health dovetail through ongoing integrated support
- Search for a job for each person on an individual basis, rather than finding generalised job vacancies before putting people into them
- Not place a limit on the amount of time that people can be supported once they gain employment, to ensure that the job is a good match and the person is able to sustain employment.
Cost is often the flipside of quality – services set up at less than £4,000 per client have been unable to achieve the fidelity points above and their outcomes have been negatively affected.
Characteristics of the IPS family of services
IPS in secondary care, primary care and NHS Talking Therapies
These services are funded primarily by NHS England, with additional funding provided for implementation support from IPS Grow and staff training and development from Centre for Mental Health. The services aspire to high fidelity and the majority have achieved it, along with success rates of between 30% and 40% job outcomes.
IPS (PC)
IPS (PC) services are funded by DWP for people receiving health services from primary care. Typically, referrals will be for people with common mental health problems, disabilities and other long-term conditions. The IPS services take referrals for anyone with a health condition that creates a barrier to work. Referrals may come from GP surgeries, social prescribers or Job Centres. Time limits apply to the length of support that can be offered, and there is minimal, if any, ongoing integration of health support with employment support. These services do not achieve the quality of high fidelity and clients may find that the support offered is too ‘light-touch’ to be effective. Most have not yet been assessed for quality and fidelity.
WorkWell
The new WorkWell contracts will fund providers to support people referred by Job Centres who have very recently become unemployed or are still in work, but need help to retain their employment. WorkWell is designed to be ‘low intensity’ support, which again means that quality and fidelity will be low. It remains to be seen whether a lower cost alternative to IPS will be successful. Sheffield Hallam University’s evaluation of Manchester’s Working Well Early Help programme (a model which informed the new WorkWell service) concluded that it was helpful for people who were off sick from work and needed support to get back into their existing job, but it was less effective than expected in moving people from unemployment into paid work.
IPS-AD
In contrast, IPS teams established in Drug and Alcohol services, funded by the Office of Health Improvement and Disparities, have been rated as very high fidelity and achieve an average of over 40% of clients entering and sustaining paid work. IPS-AD teams have modelled daily integration with addiction treatment teams, resulting in high-quality personalised support into lasting employment.
Universal Support IPS
The newest member of the IPS family is still to arrive. This will be IPS for people in the ‘support’ group of people on out-of-work benefits, whose health problems are a significant hindrance to finding and keeping work. But many people in this situation want to work, and as we have seen in people living with severe mental illness, can do so very successfully.
A foundation of the IPS model is that participation is never compulsory or a condition of receiving benefits. It helps people into the right kind of work at the right time for them. As long as Universal Support does not become ‘mandatory IPS’ or force people to take the jobs on offer or lose their benefits, it may succeed where previous Work and Health Programmes have fallen short.
Centre for Mental Health will watch the progress of these different types of IPS with interest. Through the application of the fidelity scale, and quality staff development, the aim must be to ensure that wherever and however IPS is provided, it will always be delivered effectively with the person’s health and employment needs being carefully considered in the search for appropriate placement and support in paid work. We must not allow the good reputation that traditional IPS has built through years of high fidelity delivery to become tarnished by cheap imitations.









