A public health model for mentally healthier integrated care systems
Ed Davie
The Covid-19 pandemic is being accompanied by a sharp rise in demand for mental health services. Whilst high quality clinical services are vital in addressing rising needs, the size and nature of the challenge means that treatment alone cannot manage this crisis.
Better together: A public health model for mentally healthier integrated care systems outlines how integrated care systems can adopt a public health model to use their budgets, powers and influence to support better mental health outcomes for all.
Involving all NHS bodies and local authorities in 42 areas covering the whole of England, integrated care systems have an increasingly important role to play in organising health and care and addressing the wider factors that influence people’s health.
To support better mental health, integrated care systems must focus on reducing poverty and inequality whilst improving the environment and providing tailored support for people with the highest risks of mental illness.
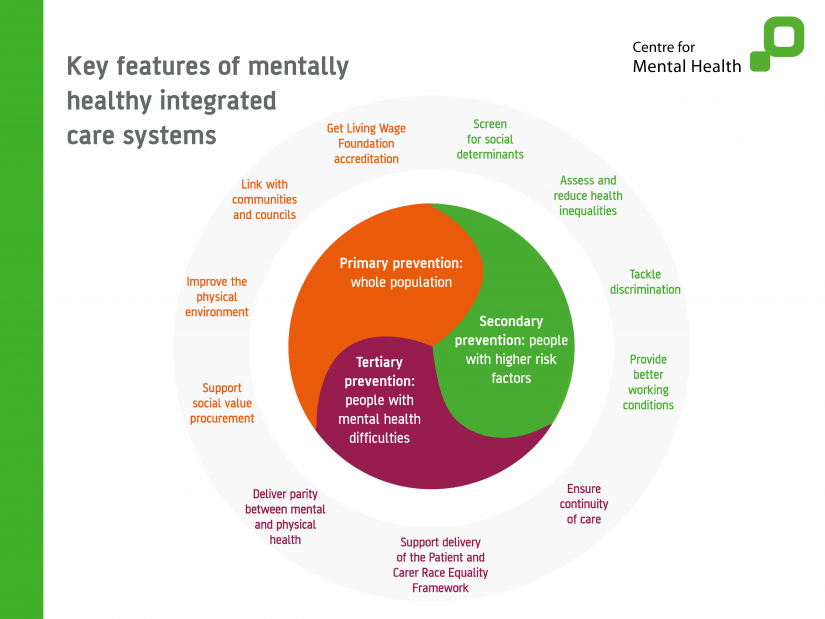
The briefing highlights three equally important aspects to a public health model of preventing mental ill health:
- Primary prevention: supporting whole population mental health, for example by getting Living Wage Foundation accreditation and reducing air pollution
- Secondary prevention: supporting people with higher risk factors for mental illness, by tackling discrimination and screening for social needs, for example
- Tertiary prevention: supporting people with mental health difficulties, for example by delivering parity between mental and physical health and ensuring continuity of care for those leaving prison.
Adopting a public mental health model based on addressing these factors will reduce risks and demand whilst improving people’s mental health outcomes. This briefing provides a valuable framework for creating mentally healthier integrated care systems.
Want to hear more about this?
We’re building a network of people working in integrated care systems who are interested in creating better mental health outcomes in their communities. Join the network.








