Improving the physical health of people with severe mental illness
Jan Hutchinson
People living with severe mental illness face a 15 to 20 year shorter life expectancy than the general population. This is largely due to physical illnesses that could be prevented or treated.
One of the ways to tackle this unacceptable inequality is by ensuring everyone with severe mental illness is supported to access an annual physical health (PHSMI) check. This report with Equally Well UK, commissioned by NHS England, explores how new investment has been used around the country to improve outreach services and increase uptake of the PHSMI check.
Reaching out illustrates the barriers that can prevent people from accessing their physical health check, such as finding morning appointments challenging due to drowsiness from medication, or distrust of NHS services due to previous experiences (including compulsory treatment). It highlights the importance of coproduction in designing outreach initiatives to remove these barriers.
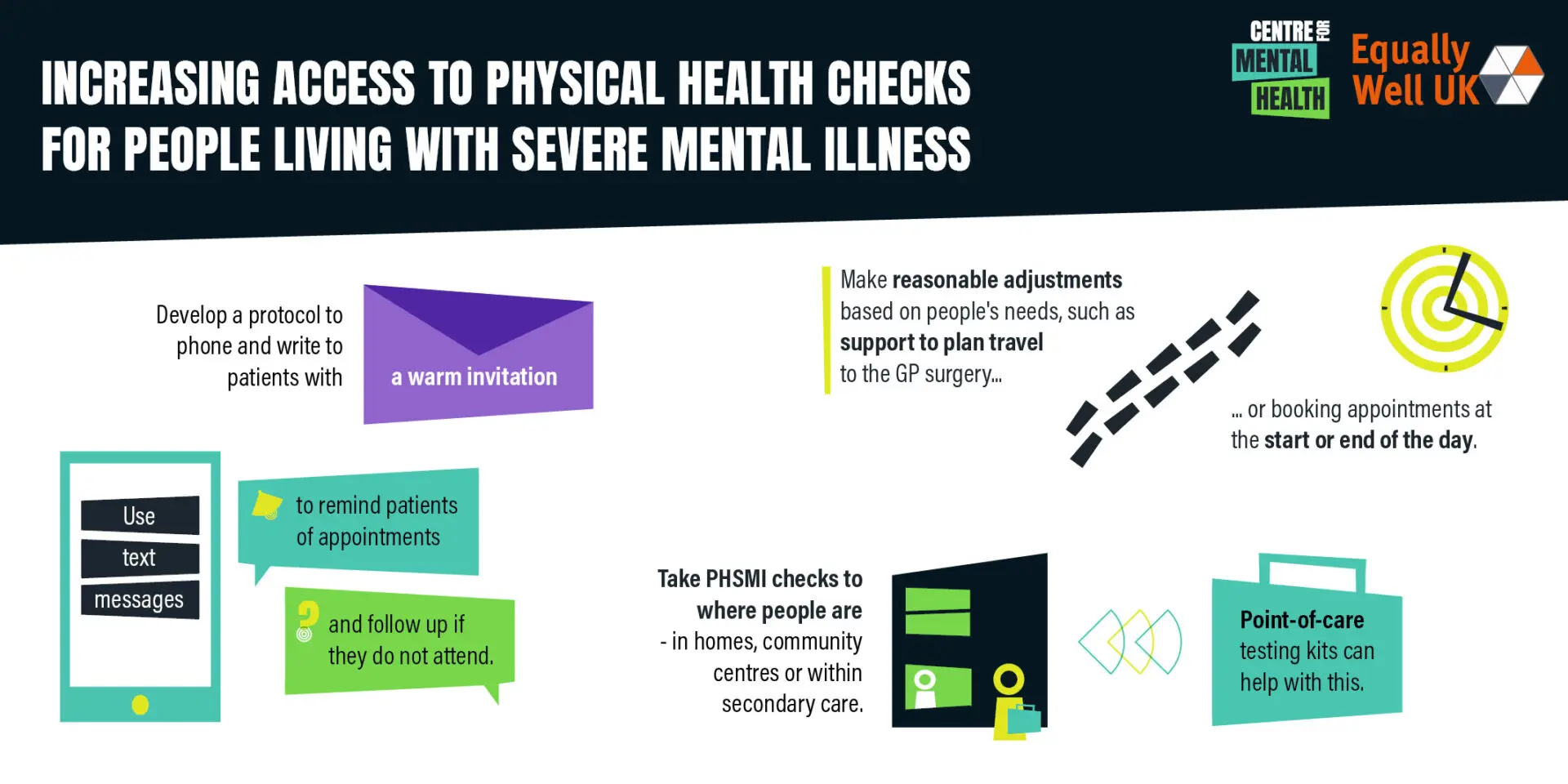
It also contains a handy information sheet with key tips on widening access to physical health checks for people with severe mental illness, such as using point-of-care testing kits to take PHSMI checks to where people are, or supporting people with travel to the GP surgery.
The report calls for outreach to be part of a wider strategy to improve the physical health of people living with severe mental illness and reduce the mortality gap.